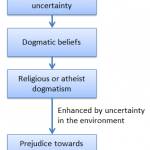
We all hold beliefs that are not provable, and defining when these beliefs cross the line and become psychotic delusions is not easy. It’s clear that such a line does exist, however: every town has its share of people whose religious beliefs fall sufficiently far outside the conventional that they are declared psychotic.
In popular imagination, at least, psychotic delusions often have a religious component. In reality, many psychotic delusions are not religious. However, many delusions involve hallucinations or mind control by unseen agents, and so it’s not too surprising that those who experience them fold them into their religious background. The religious beliefs don’t trigger the psychosis, but they become enmeshed within it.
But do religious beliefs help or hinder those with delusions?
Sylvia Mohr, at the University Hosptial of Geneva in Switzerland, took a look at over 200 psychiatric outpatients at two mental health institutions – one in Geneva and the other in Trois-Rivières, Québec. Half of them had frequent psychotic delusions, and 38 (around one in six of the total sample) had delusions with religious content.
She found that religious nature of their delusions did help some patients to cope. For some, who believed they were being persecuted demons, belief in their god or guardian angel gave them comfort and strength to deal with their condition. This is what one patient said:
The auras say “we will catch him” and “we will kill him,” and they make me feel external pain. At the beginning, I was hopeless and I believed that the auras were strong and superior. I spoke to the priest about the auras, and he helped me to find the courage to fight. God loves me and comforts me. With the help of God, I am winning against the auras. They cannot hurt me anymore, and they are inferior. I don’t speak about this to the psychiatrist, because it is very personal. I do not have a mental disorder, but a physical illness due to the auras, so I take the medication”.
For one patient, who believed he was being controlled by supernatural entities, turning to his priest helped them to understand that his delusion was an illness. Others had similar tails to tell.
However for most patients (55%, in fact), the religious component of their delusions actually made their condition more serious. This was especially the case for those suffering from self-delusions – thinking that they are somebody else. The delusion that you are John the Baptist seems to make it harder to cope with your disease than the delusion that you are Napoleon!
Patients with delusions – and especially those with religious delusions – tended also to be more religious than those. And this is where their real problems begin.
For one thing, despite being more religious, patients with religious delusions actually engage in fewer group religious activities and receive less support from their religious communities than do patients with non-religious delusions. That’s presumably because their religious communities find these religious delusions particularly disturbing.
These patients also are more likely to find that their religion brings them into conflict with psychiatrists and others who are trying to provide mental health support. In fact, one in four of them have come to believe that their religion does not allow them to take antipsychotic medication.
So religion is a mixed bag when it comes to psychosis. For some, it provides solace. For others, however, it increases the danger that they will sink further into their own delusions – a problem exacerbated by the fact that they are shunned by their religious colleagues.For these patients, their religion is more often a burden than a support.
![]() Mohr, S., Borras, L., Betrisey, C., Pierre-Yves, B., Gilliéron, C., & Huguelet, P. (2010). Delusions with Religious Content in Patients with Psychosis: How They Interact with Spiritual Coping Psychiatry: Interpersonal & Biological Processes, 73 (2), 158-172 DOI: 10.1521/psyc.2010.73.2.158
Mohr, S., Borras, L., Betrisey, C., Pierre-Yves, B., Gilliéron, C., & Huguelet, P. (2010). Delusions with Religious Content in Patients with Psychosis: How They Interact with Spiritual Coping Psychiatry: Interpersonal & Biological Processes, 73 (2), 158-172 DOI: 10.1521/psyc.2010.73.2.158
 This article by Tom Rees was first published on Epiphenom. It is licensed under Creative Commons.
This article by Tom Rees was first published on Epiphenom. It is licensed under Creative Commons.